News
A Gut Feeling: How our brains are directly linked to our guts
We casually refer to a “gut feeling” and “butterflies in our stomach.” But, there is scientific evidence that connects stress to digestive disorders, thereby validating those “gut-wrenching feelings” that cause worry in our minds and irritation in our bellies.
The connection between the brain and gastrointestinal system is intricate and undeniable. One affects the other, and the connection goes both ways – a troubled mind can leave the stomach “in knots,” and conversely, a “bad belly” can cause stress, anxiety or depression. With so many daily stressors in life, it’s no wonder the National Institute of Diabetes and Digestive and Kidney Diseases estimates 60 to 70 million Americans are affected by digestive diseases. It’s true that people or situations that make you mad, frustrated or sad can truly “give you heartburn.”
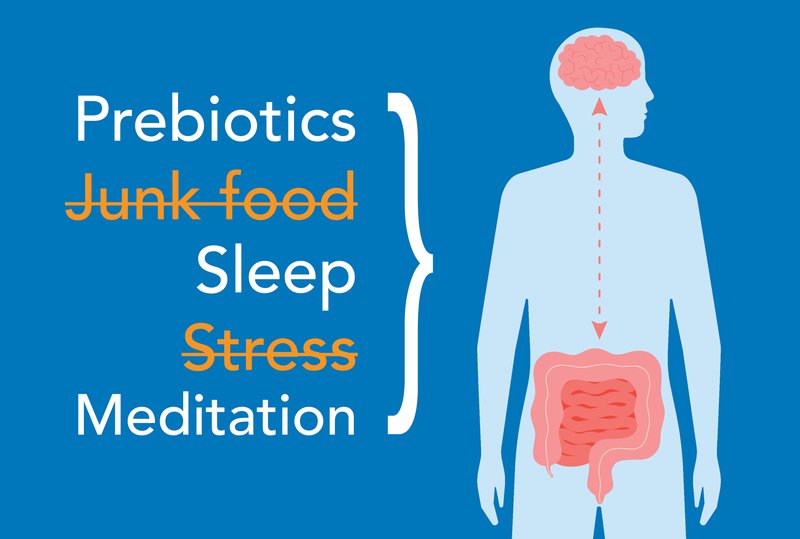
All puns aside, real studies have shown that stressful life events can cause – or worsen – stomach disturbances like bloating, constipation, diarrhea and heartburn. They can also exacerbate the symptoms of ongoing digestive disorders like irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD) and inflammatory bowel disease (IBD). That’s because, like the brain, the belly is full of nerves that make up the enteric nervous system (ENS), also known as the “second brain.” The gut contains the largest area of nerves outside the brain, and the two share many of the same nerve connections, including the vagus nerve, which is part of the parasympathetic nervous system and is responsible for our mood, stress response and digestion.
The vagus nerve sends information from your gut to your brain, and when the nerve is working properly, the brain sends back the right response immediately. For example, if you eat something spicy that causes some intestinal inflammation, the vagus nerve sends a message to the brain that there’s some inflammation. The brain then triggers a biologic response in the intestines to decrease the inflammation. A weak or damaged vagus nerve can disrupt these important lines of communication, so it’s important to maintain a strong vagus nerve.
How do we strengthen a nerve some of us didn’t even know existed? An increasing number of studies show that relaxation techniques like deep breathing, yoga and meditation help support the vagus nerve, thereby improving communication between the brain and the gut, and promoting good digestion.
“Worrying about your gastrointestinal symptoms, the underlying causes and the effects they have on your day-to-day quality of life can be very cyclical,” said Allisa Corsbie, NP-C, a gastroenterology and hepatology specialist at Colorado Mountain Medical. “I’m such a proponent of maintaining positive mental health in order to promote a healthy gut.”
The link between the gut and the brain is further influenced by the gut's microbiome, which is made up of trillions of microorganisms that can be both beneficial and harmful within and outside of the gastrointestinal tract. Critical to health and wellbeing, the microbiome can be disrupted by poor mental health, diet, infections and antibiotics.
Many of our brain’s chemicals begin in the gut, therefore, there’s actually a science to “following your gut instinct.” In fact, 95 percent of our serotonin supply is created by gut bacteria, as are other neurotransmitters like dopamine, norepinephrine, acetylcholine and GABA, which directly affect our mood, anxiety, concentration and motivation. Since these chemicals are so important to our mental health, it can be assumed that improving your gut health could improve your mood.
Conversely, when you become nervous or anxious, your body releases epinephrine/norepinephrine, which enters the digestive system and can inhibit digestive activity. The microorganisms that live along the gut can be affected by these chemicals, thereby resulting in imbalances that cause conditions like IBS, GERD and IBD.
Of course, there is also the issue of what we put in our stomachs when we’re under stress. “Comfort foods” can appeal to what the brain thinks will make someone feel better in the moment, but they’re often unhealthy and eaten in excess. People under stress may also drink more alcohol or smoke more often. All of this can lead to heartburn, acid reflux, and if not treated, can cause ulcers.
“Thankfully, our lifestyle choices can be modified once we identify dietary choices and behaviors that play a role in disrupting the microbiomes in our gut,” said Corsbie.
Hence, another reason to talk about your feelings with a professional or trusted confidant – studies show that psychologically-based interventions lead to greater improvements in digestive symptoms compared with only conventional medical treatment. Stress is inevitable, but adopting coping techniques can help you manage the stress, thereby preventing not only stomach issues but also more dangerous conditions like obesity, heart disease and stroke.
“It is important to identify what works for you,” said Corsbie. “Prioritizing adequate sleep is essential as it is a time for restoration and the release of hormones that help with immune function and cellular repair. Exercise releases endorphins and can help you lose weight, which has been shown to reduce pressure on your abdomen. Others may need to relax with techniques such as stretching, deep breathing, meditating, taking a relaxing walk or just sitting in the sun. Alone time, catching up with a friend, or joining a group activity can all serve different purposes for fulfilling mental health needs. Keep trying until you find something that works for you.”
Certain foods can boost gut and mental health as well. Fiber, for instance, has been shown to improve memory and overall mood. It also decreases inflammation by supporting microorganisms in the gut. Protein contains nitrogen, which limits the amount of bad bacteria in the microbiome. Eating protein also produces serotonin, which positively affects your mood.
“Studies have shown a positive impact on anxiety and depression when consuming a healthy diet rich in pro- and prebiotic-containing foods,” said Corsbie. “Try to incorporate foods that contain natural prebiotics, which nourish gut bacteria. A few examples include oats, flaxseed, sunflower seeds, walnuts, bananas, legumes, garlic, onion, dates and figs. Dairy, processed meats and artificial sweeteners can cause certain gut bacteria to flourish. These bacteria are associated with an increased risk of inflammatory and cardiovascular conditions.”
From the brain to the belly, there are an incredible number of dynamic functions taking place in our bodies every day. We can support them with a healthy diet, sleep, exercise and stress management. After all, an upset mind can lead to an upset stomach—and vice versa—so take care of both.
More News
-
More

The Benefit of Doing Hard Things
How Creating Resiliency Impacts Long-Term Health I had just returned from my first Hyrox, a fitness race...
-
More

Spring Is in the Air, And So Are Allergens—How to Combat Spring Allergies
For some of us, April marks the end of the ski season. For allergy specialists like me, it means the beginning of a...
-
More

The 3 Cs of Measles
Recent news reports on measles outbreaks have brought the once-dormant disease to the forefront of many...





